Quality of life (QoL) is a subjective measure of a patient’s health perceptions and functional status.1 AF, with its unpredictable arrhythmia episodes, impairs the quality of everyday life by imposing physical, mental and social limitations. Additionally, patients experience worry and anxiety about financial concerns due to loss of workdays and the cost of AF management. Moreover, although rarely life-threatening, AF is associated with increased morbidity and mortality, predominantly through an increased risk of thromboembolic events and left ventricular dysfunction, thereby increasing the likelihood of healthcare resource utilisation such as hospitalisation and emergency room visits.2
The management of AF is centred on control of arrhythmia, and stroke prophylaxis. Catheter ablation for AF has emerged not only as a widely practised strategy to accomplish long-term sinus rhythm in drug-refractory AF cases, but also as a first-line therapy especially in younger patients with paroxysmal AF and minimal structural heart disease.3–5 The techniques, as well as the safety and efficacy of the ablation procedure in AF, have improved dramatically since they were first introduced in 1998.6 Several trials have reported significant advancement in QoL and reduction in healthcare utilisation following catheter ablation utilising advanced-generation technology.1,2,7–23 The aim of this review is to analyse the available evidence on this subject.
Impact of Catheter Ablation on QoL in AF Patients
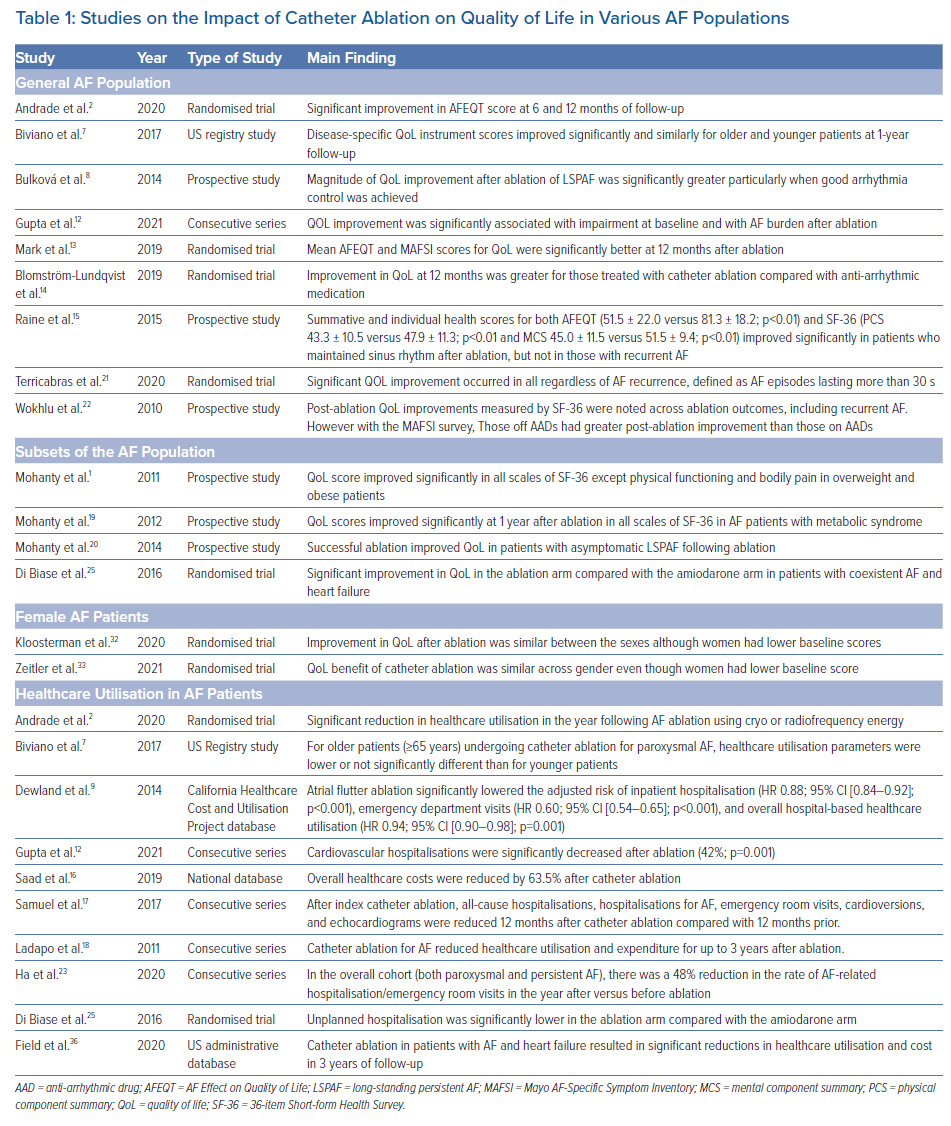
Eliminating subjectivity (and thereby bias) in medicine was the focus of modern-day clinical research until recently. However, the emphasis is gradually shifting towards patient-reported outcomes and QoL.24 Several generic and disease-specific tools are used to measure QoL, and the majority of the studies assessing QoL in patients undergoing catheter ablation have shown significant improvement in this metric (Table 1).
In a consecutive series of AF patients undergoing catheter ablation, Wokhlu et al. reported post-ablation improvement in QoL regardless of ablation success.22 QoL improvement in patients with post-ablation recurrence was attributed to plausible causes such as a reduction in symptom burden, improved efficacy of drugs that were previously ineffective, and a placebo effect of the ablation procedure, among others.22 They also documented the superiority of AF-specific assessment (Atrial Fibrillation Effect on Quality of Life; AFEQT) over the generic QoL questionnaire, the 36-item Short-form Health Survey (SF-36), which most likely was not an appropriate metric to measure AF-related QoL.22
Raine et al. utilised both SF-36 and the AFEQT questionnaire to assess QoL in patients undergoing catheter ablation for AF.15 They reported improvement in QoL scores only in patients (of all AF types) who maintained sinus rhythm after ablation. Additionally, they reinstated the higher sensitivity of AFEQT over SF-36 in capturing changes after catheter ablation.15 Although the authors observed QoL improvement only in arrhythmia-free individuals, because of discontinuous arrhythmia monitoring the study was not able to rule out asymptomatic episodes in patients with sinus rhythm.15
In another prospective analysis, patients with long-standing persistent AF (LSPAF) with worse baseline QoL compared with the patients with paroxysmal AF had greater improvement in post-ablation QoL, particularly those who remained in sinus rhythm off anti-arrhythmic drugs.8 A shorter history of AF, younger age and presence of LSPAF were found to be independent predictors of QoL Improvement.8
Two multicentre US registry studies reported comparable improvement in post-ablation AF-specific QoL scores in patients older and younger than 65 years, at 1-year follow-up.7 In 2,204 randomised patients in the CABANA trial, both the AFEQT and MAFSI (Mayo AF-Specific Symptom Inventory) mean scores were more favourable in the catheter ablation group than in the drug therapy group.13 The CAPTAF randomised trial reported similar findings.14
A secondary analysis of the STAR AF II trial demonstrated a 92% reduction in AF burden following catheter ablation and a direct association of statistically significant improvement in QoL with decrease in AF burden at 18 months following the procedure.21 The QoL improvement was detected regardless of AF recurrence, defined as AF episodes lasting >30 seconds.21 The CIRCA-DOSE randomised trial also reported the same.2 Patients free of any atrial tachyarrhythmia recurrence had a significantly greater improvement in AFEQT score compared with those with tachyarrhythmia recurrence.2 Another consecutive series documented association of QoL improvement with residual tachyarrhythmia burden following catheter ablation.12
Catheter ablation has also been shown to positively impact QoL in subsets of AF patients with other comorbidities. In a prospective series of 660 normal versus high BMI patients, we observed significant increase in QoL scores in high BMI patients only.1 Furthermore, patients with successful ablation had more positive change in QoL compared with those with failed ablation.1 In another study including AF patients with metabolic syndrome, the QoL improvement was observed to be greater in patients with metabolic syndrome versus without.19 In a later series with asymptomatic LSPAF patients, successful ablation was shown to be associated with substantial betterment in QoL scores.20 In the AATAC randomised trial, the Minnesota Living with Heart Failure questionnaire was used to assess the change in QoL in AF patients with congestive heart failure undergoing catheter ablation versus those remaining on amiodarone.25 Compared with the drug group (and with both cohorts having similar QoL scores at baseline), the ablation arm had significantly better QoL at follow-up.25
Another subset of AF in terms of QoL impairment is worth mentioning. Many trials have shown that women with AF have lower baseline QoL than men.26–31 The AXAFA-AFNET 5 trial reported similar improvement in QoL following catheter ablation, across gender.32 In a substudy of the CABANA trial population, catheter ablation was shown to be superior to drug-based therapy for improving QoL in women.33
Impact of Catheter Ablation on Healthcare Utilisation
According to a cross-sectional study using the Nationwide Inpatient Sample database for the years between 2000 and 2010, a total of 3,960,011 hospitalisations for AF as the primary discharge diagnosis were reported in the US.34 The contemporary costs of managing AF have been estimated to account for 1.0–2.7% of total annual healthcare expenditure, with a significant proportion of these expenses attributed to the direct costs associated with hospitalisation, emergency room visits and the provision of acute care.2 In 2010 the AF-specific cost was reported to be US$6.0 billion, consisting of US$2.3 billion for inpatient admissions with AF as the primary diagnosis and US$3.7 billion for outpatient care.35 Many independent trials have reported a significant reduction in healthcare resource utilisation following AF ablation (Table 1).
The CIRCA-DOSE randomised trial reported a reduction of 75% in cardioversion, 62% in emergency room visits, 43% in hospitalisation and 86% in anti-arrhythmic drugs use following catheter ablation using either radiofrequency or cryo energy, in paroxysmal AF patients.2 In a consecutive series, Gupta et al. documented significant reduction in cardiovascular hospitalisation following AF ablation.12 In a retrospective cohort of patients from the Brazilian private healthcare system, overall healthcare cost was shown to reduce by 63% after catheter ablation compared with before.16 Biviano et al. showed comparable reduction in healthcare utilisation (hospitalisation and emergency room visits) following catheter ablation in both older and younger patients with a cut-off age at 65 years.7
In a large real-world population of 33,000 patients with a diagnosis of atrial flutter, catheter ablation was shown to significantly reduce the adjusted risk of inpatient hospitalisation, emergency room visits and overall hospital-based healthcare utilisation.9 Samuel et al. demonstrated reversal of healthcare resource utilisation at 2 years following catheter ablation to lower than pre-ablation levels in 1,556 AF patients.17 The rate of all-cause admissions and AF or atrial flutter hospitalisation and emergency room visits increased significantly over the 24-month period prior to ablation and subsequently decreased below pre-procedure levels throughout the 24 months following the ablation procedure.17
In another study on healthcare utilisation in the general and the Medicare populations, compared with the 6 months prior to ablation, there were significant reductions in the number of outpatient appointments, inpatient days, drug treatment, and emergency room visits in the total study population and in the subset ≥65 years, at 3 years after the ablation procedure.18 In the AATAC study, unplanned hospitalisation was significantly lower in the ablation arm in patients with coexistent AF and heart failure.25 Similar findings were reported by Field et al. at 3-year follow-up in patients with AF and heart failure undergoing catheter ablation.36 In two recently published studies, the authors showed benefits of catheter ablation in terms of healthcare utilisation and cost in both paroxysmal and persistent AF.13,23
Conclusion
Based on the above evidence, it is prudent to conclude that catheter ablation improves disease-specific QoL regardless of the ablation outcome. Furthermore, irrespective of AF type, it significantly reduces the healthcare utilisation in the post-ablation period for up to 3 years.
Clinical Perspective
- Catheter ablation improves quality of life (QoL) in AF patients, regardless of ablation outcome.
- Positive change in QoL even in the absence of achievement of sinus rhythm is probably due to reduction in arrhythmia burden and improved efficacy of drugs that were previously ineffective.
- Significant reduction in healthcare utilisation such as hospitalisation and emergency room visits following catheter ablation has also been well documented.
- When determining the priority of catheter ablation in AF patients, the aforementioned benefits should be considered along with the success rate of the procedure in achieving arrhythmia-free survival.