Dr Stanley Nattel from Montreal, Canada, began with an overview of the history of the term atrial cardiomyopathy and its use in conjunction with atrial fibrillation (AF), setting the stage for their present-day definitions.
The European Heart Rhythm Association (EHRA), the Heart Rhythm Society (HRS), the Asia Pacific Heart Rhythm Association and the Latin American Society for Cardiac Stimulation and Electrophysiology attempted to standardise the definition, characterisation and clinical implications of the term atrial cardiomyopathy in 2016. In the resulting consensus document, atrial cardiomyopathy was defined as “any complex of structural, architectural, contractile or electrophysiological changes affecting the atria with the potential to produce clinically relevant manifestations”.2
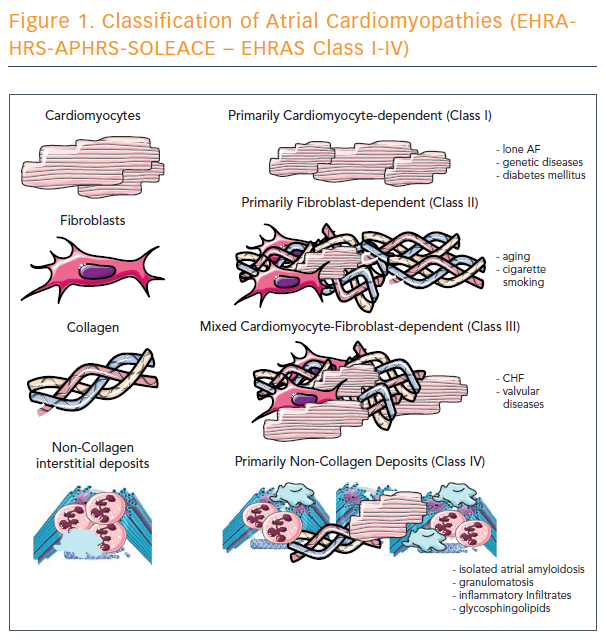
The consensus document also produced definitions for four classes of atrial cardiomyopathies (see Figure 1). This histological classification has many limitations.
However, it is a useful beginning that will help clinicians consider the histopathology of atrial cardiomyopathy in a more organised way. Dr Nattel believes that it will be possible in the relatively short term to create a more meaningful classification and to use it to define clinically relevant predictive factors and therapeutic decisions. The next step will be to test the classification to evaluate whether it can be used to guide clinical care in practice.
Atrial cardiomyopathy is an evolving concept. There is evidence that consideration of atrial cardiomyopathy may add value to patient management. A more clinically relevant classification considering aetiological factors and indices of electrical, mechanical and structural remodelling would help in identifying practical applications of the concept.