In 1941, Mahaim and Winston described the histology of anomalous connections that arise from the AV node and insert into the right ventricle.1 This was the first description of nodoventricular or so-called Mahaim accessory pathways. Accessory pathways with decremental conduction properties that connected the atrium to the right bundle branch (RBB) were subsequently mapped mainly at the lateral aspect of the tricuspid annulus, and thus the term atriofascicular was also adopted.2-4 We know now that decrementally conducting connections can be between the right atrium or the AV node and the right ventricle in or close to the RBB.5-7 Thus, although they are anatomically distinct from the initially described nodoventricular pathway, they present with similar electrocardiographic and electrophysiological characteristics and the term ‘Mahaim’ has been adopted to describe pathways with the following features:
- Baseline normal QRS or different degrees of manifest preexcitation with left bundle branch block morphology;
- Programmed atrial pacing leading to obvious manifest preexcitation following an increase in A-V interval along with shortening of H-V interval at shorter pacing cycle lengths; and
- Right bundle electrogram preceding His bundle activation during anterograde pre-excitation and supraventricular tachycardia (SVT).
Although such pathways are rare, their unique properties as well as the still unanswered questions about their true nature, make them particularly interesting from an electrophysiological point of view.8
Electrocardiographic Features
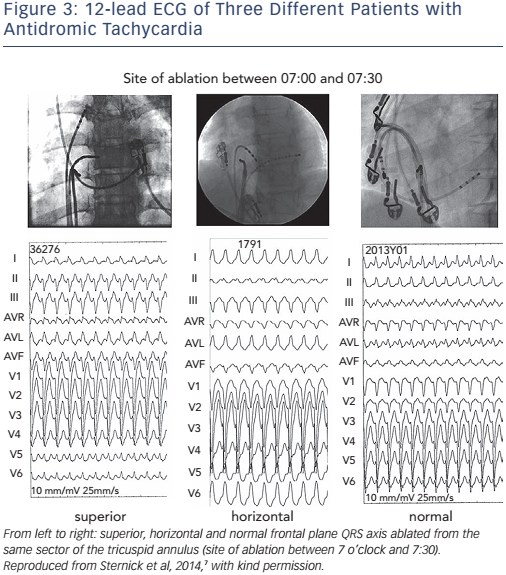
ECG During Sinus Rhythm
During sinus rhythm overt pre-excitation is usually absent (see Figure 1). Only subtle ECG abnormalities, such as an rS pattern in lead III, absence of septal Q waves in leads I and V6, and terminal QRS slurring or notching, suggest the presence of Mahaim conduction.9,10 However, patients with short, rapidly conducting fibres may have typical pre-excitation.10
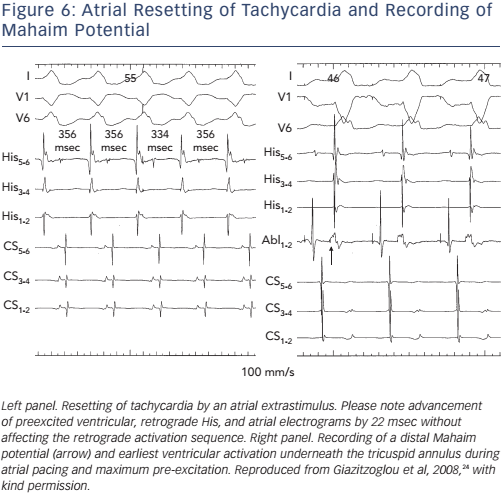
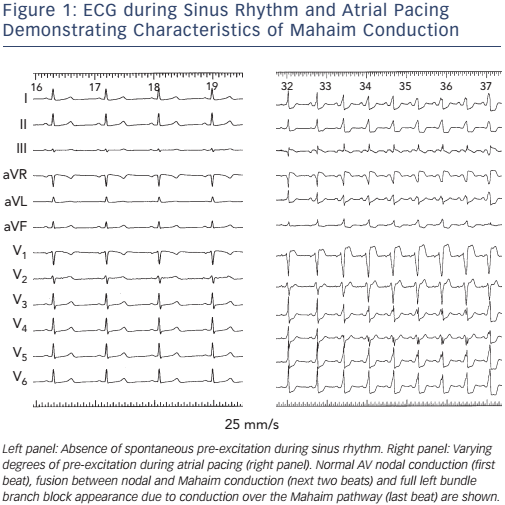
ECG during tachycardia
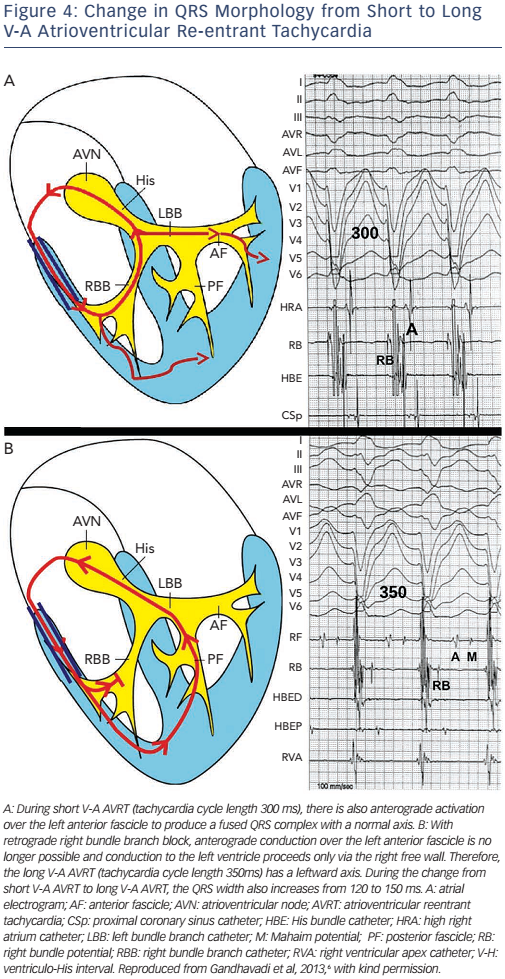
Although, typically, antidromic atrioventricular reentrant tachycardia over a Mahaim fibre has a left bundle branch (LBBB) morphology (see Figure 2), various QRS patterns and axis may occur (see Figure 3).6,7 It seems that these pathways insert into or near the RBB, and variations in the frontal plane axis can be explained by the location of the exit of the RBB and a variable degree of fusion of ventricular activation between anterograde conduction over the pathway and, following retrograde invasion into the RBB, partial anterograde left ventricular activation over the left-sided conduction system, especially the anterior fascicle (see Figure 4). The various QRS patterns and rate changes seen during the change from short to long V-A tachycardia can be explained by the mode of retrograde conduction over the bundle branch system.6,7
Electrophysiological Properties
Nodoventricular or Atriofascicular?
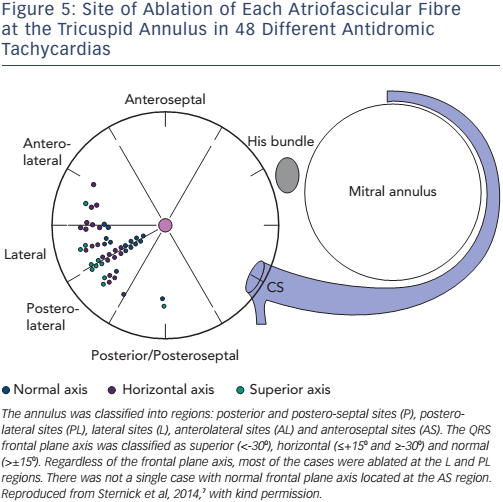
Although the first case of this arrhythmia was studied electrophysiologically by Wellens and published in 1971, and considered to be based on a nodo-ventricular pathway,11 with the advent of surgical and then catheter ablation in the 1980s, it was discovered that most fibres with Mahaim conduction characteristics originated at the lateral aspect of the tricuspid annulus, and the term atriofascicular pathway was adopted.2-5,12-17 However, posteroseptal locations could also be found,7,14 and true nodoventricular fibres have been identified (see Figure 5).1,14,16 In addition, some of these pathways, so-called ‘short’ as opposed to ‘long’ Mahaims, may insert at the ventricle near rather than in the RBB.5-7,18 Thus, pathways with Mahaim characteristics can be atriofascicular, atrioventricular, nodofascicular and nodoventricular, depending on their variable proximal and distal insertions.
Origin
The electrophysiological properties of Mahaim pathways are not uniform, and this may reflect the diversity of the limited histology findings.5,18 It seems that most, but not all, of these pathways represent duplications of the AV nodal conducting system and contain nodal tissue, and their association with the R3-2Q mutation in PRKAG2 has been considered as an indication that this gene is involved in the development of the cardiac conduction system.19 They may display spontaneous or post-ablation automaticity,13,20 may respond to adenosine but not to verapamil,21 and their properties may depend on their location and insertion site.5,13
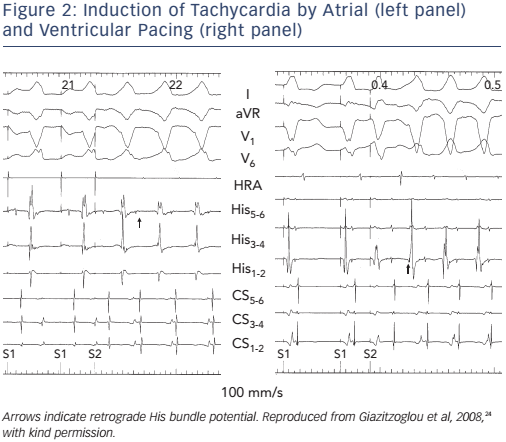
Catheter Ablation
Mahaim pathways are typically decremental and conducting only anterogradely. However, retrogradely conducting nodoventricular pathways have been described.22,23 Whether such pathways are classified as ‘true’ Mahaims is a matter of terminology rather than essence. Catheter ablation is accomplished by identifying the proximal and distal insertions and, ideally, the recording of a proximal pathway potential at the tricuspid annulus or a distal one on the right ventricular free wall (see Figure 6).5,13-17 Pathway potential recording may be facilitated during atrial pacing. Since most of the Mahaims are mapped on the lateral tricuspid annulus or right free wall underneath the valve, the use of supportive long sheaths that stabilise the ablating catheter may be very helpful.24 Rare true nodoventricular pathways may also be ablated with preservation of AV nodal conduction.25
Conclusion
Mahaim pathways are decrementally conducting connections between the right atrium or the AV node and the right ventricle in or close to the right bundle branch. They can be atriofascicular, atrioventricular, nodofascicular and nodoventricular, depending on their variable proximal and distal insertions. Catheter ablation is accomplished by identifying the proximal and distal insertions and, ideally, the recording of a proximal pathway potential at the tricuspid annulus or a distal one on the right ventricular free wall.
Clinical Perspective
- Mahaim pathways are decrementally conducting connections between the right atrium or the AV node and the right ventricle in or close to the right bundle branch.
- The baseline QRS is normal or displays different degrees of manifest pre-excitation with left bundle branch block morphology.
- Programmed atrial pacing leads to obvious manifest preexcitation following an increase in A-V interval along with shortening of H-V interval at shorter pacing cycle lengths, and right bundle electrogram preceding His bundle activation during antegrade pre-excitation and reentrant tachycardia.
- Catheter ablation is accomplished by identifying the proximal and distal insertions and, ideally, the recording of a proximal pathway potential at the tricuspid annulus or a distal one on the right ventricular free wall.