Sudden cardiac death (SCD) is a major public health concern worldwide, accounting for 50 % of cardiovascular mortality.1 Reduced left ventricular ejection fraction (LVEF) is presently used to identify patients at high risk for primary prevention using implantable cardioverter defibrillator (ICD) therapy, but currently only a minority of patients meeting the criteria for prophylactic ICD receive lifesaving therapies from the device.2 On the other hand, in absolute numbers, the majority of SCDs occur among individuals considered to be at low risk based on LVEF, which has promoted vast interest in developing additional risk markers in order to identify these patients before the fatal event. As the immediate mechanisms of SCD are primarily electrical, much of the research has focused on different electrocardiographic risk markers.3
Physiological Bases of T-wave Alternans
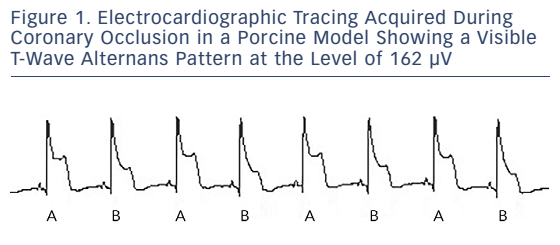
Microvolt T-wave alternans (TWA), a subtle beat-to-beat fluctuation in the morphology and amplitude of the ST-segment and T-wave, has emerged as a promising tool to estimate risk of mortality and SCD in patients with cardiac disease. It reflects spatiotemporal heterogeneity of repolarisation that stems from beat-to-beat alterations in intracellular calcium handling, which is reflected in the shape and duration of the action potential at the level of cardiac myocytes (see Figure 1). These local differences in the repolarisation of the neighbouring myocardial regions can ultimately predispose the individual to lethal arrhythmias such as ventricular tachycardia or ventricular fibrillation.4
Several physiological as well as pathological conditions can alter the levels of TWA, and the magnitude of TWA and risk of arrhythmias often concur. Conditions that are associated with increased risk of ventricular arrhythmias (e.g. increased heart rate, ventricular premature beats, coronary ischaemia and adrenergic stimulation) also amplify TWA, and conversely, interventions such as b-blockers, sympathetic denervation and vagus nerve stimulation that reduce susceptibility to ventricular arrhythmias also cause TWA to diminish.5
T-wave Alternans Analysis Techniques
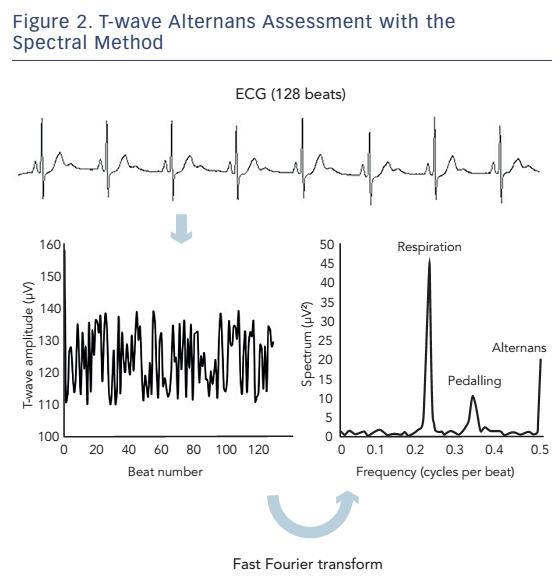
To analyse the microvolt level alternations in the ST-segment and T-wave, special equipment and/or software are needed. Several analysis methods have been proposed over the past three decades,6,7 but two of the most widely used TWA analysis techniques in clinical studies are the spectral method8 and the modified moving average (MMA) method.9 Both of these methods perform similarly in terms of risk prediction,5,10 but there are significant differences in their implementation and interpretation. The spectral method was first described nearly three decades ago.11 It requires the patient to achieve a target heart rate of 105–110 beats per minute for a period of time using a specialised exercise protocol, pharmacological agents or atrial pacing. As opposed to the time-domain MMA method, the spectral method also requires the use of proprietary high-resolution electrodes. In the spectral method, a composite power spectrum of the ST–T segment amplitude fluctuations is formed by applying fast Fourier transform technique to the beat-to-beat series of amplitude measurements along the JT-interval in 128 consecutive QRS-aligned ECG complexes (see Figure 2). The alternans voltage is defined as the square root of the spectral power occurring at the alternans frequency (0.5 cycles/beat) after noise reduction, which corresponds to the difference in voltage between the overall average beat and either the averaged even or odd-numbered beat (i.e. half of the difference between the averaged even and odd beats). A TWA level ≥1.9 µV with sufficient signal-to-noise ratio for >2 min is defined as a positive test result, while a TWA level <1.9 µV is considered negative. However, as the spectral method requires a stable target heart rate to be achieved, a relatively large proportion (approximately 20–40 %) of tests are classified as ‘indeterminate’, either due to patient-related factors such as failure to achieve the target heart rate, excessive ventricular ectopy, atrial fibrillation or unsustained TWA, or technical problems such as noise in the recording.5
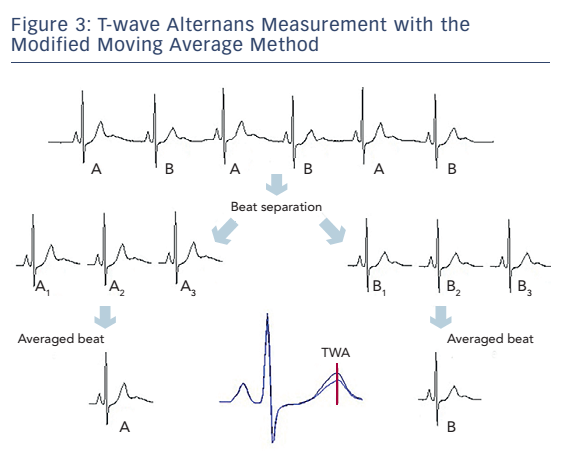
The MMA method is time-domain based, and employs recursive averaging (see Figure 3). The algorithm continuously streams odd and even beats into separate bins and creates averaged complexes for both bins. These complexes are then superimposed, and the maximum difference between the odd and even complexes at any point within the JT-segment is averaged for every 10 or 15 seconds and reported as the TWA value. The MMA method allows TWA analysis during routine exercise stress testing and also during 24-hour ambulatory ECG monitoring. No special electrodes are required using this technique, and as no target heart rate is required, indeterminate results are infrequent with the MMA method. Risk stratification is based on the peak TWA value using the MMA, and based on the study population, cut-off levels of ≥47 µV and ≥60 µV have been most commonly used to define abnormal and severely abnormal TWA, respectively.5
Prognostic Significance of T-wave Alternans
Microvolt TWA has been associated with cardiovascular mortality and SCD in numerous studies involving >14,000 individuals with both ischaemic and non-ischaemic cardiomyopathy, and with reduced as well as preserved left ventricular function. These prognostic implications were independent from several demographic and clinical factors associated with coronary artery disease and SCD, including LVEF. The spectral method has demonstrated TWA to be predictive of future cardiovascular events in >8,000 patients mostly with ischaemic heart disease and prior MI, but also in non-ischaemic cardiomyopathy and heart failure.5 In most of these studies, the risk associated with TWA has been at least two- to threefold,5 but much higher hazard ratios have been reported in some patient groups.12,13 Indeterminate test results have been shown to predict mortality at least as well as positive tests,14 thus positive and indeterminate test results are often pooled together as ‘non-negative’ TWA, and compared with negative TWA.15 In some studies, the spectral method has failed to demonstrated significant association between TWA and SCD or mortality. These negative results are at least partly due to discontinuation of b-blocker therapy before the test,16 TWA testing shortly after occurrence of MI during ongoing remodelling17,18 and using ICD discharge as the endpoint.19
The prognostic significance of the MMA method has been demonstrated in >6,000 patients with reduced and preserved LVEF, including those with coronary artery disease and prior MI.5 To date, the largest study on TWA is the Finnish Cardiovascular Study (FINCAVAS) with nearly 3,600 patients with generally preserved left ventricular function referred to routine exercise testing and analysed using the MMA method.20,21 TWA was demonstrated to be associated with increased cardiovascular mortality and SCD rates, with higher TWA values indicating greater risk. In a meta-analysis on TWA in the setting of ambulatory ECG, the group with positive TWA had over a sevenfold risk of SCD compared with those with negative TWA.22
T-wave Alternans-guiding Prophylactic Implantable Cardioverter Defibrillator Therapy
As it is well known that only a minority of patients qualifying for prophylactic ICD based on reduced LVEF ≤35 % receive appropriate therapies from the device,2 many TWA studies have tried to distinguish patients who are likely to benefit from ICD therapy from those that are not. In a pooled cohort of patients with EF ≤35 % but no ICD therapy, negative TWA was associated with a low incidence of SCD, compared with substantial SCD risk associated with both positive TWA and indeterminate TWA.23 In another study among patients with ischaemic cardiomyopathy, ICDs were associated with lower all-cause mortality rate in patients with non-negative TWA, but not in patients with negative TWA.24
However, in the Microvolt T Wave Alternans Testing for Risk Stratification of Post MI Patients (MASTER I) study (ClinicalTrials.gov ID NCT00305240), which enrolled MADIT-II (Second Multicenter Automated Defibrillator Implantation Trial) type ICD-patients with LVEF ≤30 %, risk of ventricular arrhythmias did not differ according to TWA classification, despite differences in total mortality rates.25 Similar results have been reported from a SCD-HeFT ICD-study (Sudden Cardiac Death in Heart Failure Trial; NCT00000609), in which TWA could not predict arrhythmic events or mortality.26 These results have been partly attributed to the use of ICD discharge as an endpoint, which may have underestimated the use of TWA.19 The ABCD (Alternans Before Cardioverter Defibrillator; NCT00187291) trial tested whether TWA can guide ICD therapy in patients with ischaemic cardiomyopathy and non-sustained ventricular tachycardia.27 Event rates were over twofold higher both among patients with positive TWA and positive electrophysiological study at the pre-specified 1-year endpoint. However, TWA did not predict endpoint events at 2 years.
Modification of T-wave Alterans
Pharmacological therapy with b-blockers significantly reduces the level of TWA, and can convert a positive test to negative in approximately in half of the cases.28 It is reasonable to assume, that while b-blockers may alter the development of TWA, they may similarly modulate susceptibility to ventricular arrhythmias. In a meta-analysis among patients with left ventricular dysfunction on continuous b-blocker therapy, abnormal TWA testing was associated with a fivefold risk of ventricular arrhythmic events, whereas only weak association was noted in studies on which b-blocker therapy was withheld prior to screening.16 Consequently, any TWA testing is suggested to be performed under continuous medical therapy.
Recent evidence suggests that TWA may also detect influences of non-pharmacological interventions that are known to be associated with reduced mortality rates as well. In patients with stable coronary artery disease, exercise rehabilitation reduced TWA levels both patients with and without diabetes, and during the 2-year follow-up a large proportion of the patients with positive TWA converted to negative TWA.29 Thus, TWA seems to be a method that may capture and quantify influence of mainstream clinical interventions to arrhythmia susceptibility.
Role of T-wave Alternans Testing to Guide Therapy in Clinical Practice
A large body of literature has accumulated on the potential of microvolt TWA to assess cardiovascular risk in a broad range of patients with cardiac disease beyond traditional cardiovascular risk markers or left ventricular function. There is also emerging evidence that quantitative TWA assessment might be useful to determine the efficacy of clinical interventions such as pharmacological therapy and cardiac rehabilitation.30 According to the REFINE (Risk Estimation Following Infarction Noninvasive Evaluation; NCT00399503) study, TWA testing should be performed only 10 to 14 weeks after an MI, as TWA testing in the early recovery period did not reliably identify patients at long-term risk of cardiac death.10 It should be performed on permanent medication, as halting b-blocker medication prior to TWA affects the results and does not reflect the long-lasting circumstances.16 Repeated annual testing has been also suggested, as an individual’s vulnerability to ventricular arrhythmias may change over time.19
What are the current recommendations on the use of TWA? An expert consensus statement by the American Heart Association/American College of Cardiology Foundation on risk stratification techniques on SCD in 2008 asserted that TWA may be useful for SCD risk stratification, but further information is needed on how to implement this test in clinical practice.31 Similar recommendations were provided in a consensus document focusing specifically on TWA in 2011.5 The paper concluded that it is reasonable to consider TWA evaluation when there is suspicion of vulnerability to lethal arrhythmias, but also acknowledged that there is not sufficient evidence from interventional trials to suggest that TWA can be used to guide therapy. However, the recent European Society of Cardiology guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death made no recommendations for the use of TWA in risk assessment.32
Although abnormal TWA clearly has prognostic implications, and positive or non-negative tests have been associated with substantially increased risk, currently there is not enough evidence to recommend that TWA should be used to guide therapy, such as ICD implantation. However, the EU-CERT-ICD (Comparative Effectiveness Research to Assess the Use of Primary Prophylactic Implantable Cardioverter Defibrillators in Europe; NCT02064192) study should shed more light on this important issue. EU-CERT-ICD study is a large observational study in Europe, in which extensive risk stratification tests, including TWA, are performed in a large number of patients (n=2,600) receiving prophylactic ICD aimed at studying the clinical value of non-invasive testing in predicting the appropriate ICD shocks and mortality. The EU-CERT-ICD study employs the MMA method for TWA analysis.
At present, there is not sufficient evidence to recommend TWA to be used to exclude patients with LVEF ≤35 % from prophylactic ICD therapy either, despite some studies suggesting that subjects qualifying for primary prevention ICD based on reduced LVEF but with negative TWA test are at low risk of SCD and may not benefit from ICD implantation.19 However, this approach would need to be prospectively tested before it can be recommended for clinical practice.
Conclusion
Over the last decade, TWA has remained a promising tool to assess the vulnerability to lethal arrhythmias among patients with cardiac disease to identify individuals at highest risk who may benefit from further medical interventions, especially in borderline cases. However, at present, there is not enough clinical evidence to support the use of TWA testing in routine clinical practice to guide therapy. Randomised controlled trials are needed to determine whether strategies incorporating TWA analysis alone or in combination with other risk stratification methods would enable better identification of patients at highest and lowest risk for SCD. Unfortunately, a randomised controlled REFINE-ICD trial (NCT00673842) was recently suspended because of a low recruitment rate. Therefore, it is evident that definite answer about the clinical use of TWA testing will not be obtained in the near future.
Clinical Perspective
- T-wave alternans (TWA) refers to beat-to-beat fluctuations of T-wave amplitude and morphology, and is associated clinically with impending ventricular arrhythmias and increased risk of sudden cardiac arrest.
- TWA analysis can be done as part of an exercise stress test or during a long-term (Holter) ECG recording.
- Absence of significant TWA in a patient with cardiac disease with congestive heart failure, low ejection fraction or a recent MI is associated with a low risk of sudden cardiac death.
- Within candidates for implantable cardioverter defibrillator (ICD) therapy, a negative TWA test may be useful in identifying low-risk patients who are unlikely to benefit from ICD placement. However, currently there is not enough evidence to support the use of TWA in clinical practice to guide therapy.