The coronavirus disease 2019 (COVID-19) pandemic has had a dramatic impact on the way that medical care is delivered. An overarching principle of the response to the pandemic has been to minimise hospital attendance by both patients and staff. Our hospital provides secondary and tertiary cardiac arrhythmia services to patients from across the UK. Before the pandemic, we had a well-established remote monitoring service for device patients and had successfully introduced remote follow-up of patients after catheter ablation procedures. The pandemic has meant that virtually every aspect of outpatient care delivered by our service now takes place remotely, with some significant benefits and some limitations and disadvantages. We describe our experience.
Remote Investigations
The management of many arrhythmia patients is reliant on obtaining ECGs, both at baseline and during episodes of symptoms. If an abnormality is found, a large proportion of these patients will have a discussion regarding an invasive procedure to diagnose and/or treat their underlying arrhythmia.
Holter monitoring remains a useful investigation for some patients. Where Holter monitoring was still required during the COVID-19 pandemic, these monitors were posted to patients with clear instructions provided regarding fitting and use of the Holter monitors, with patients often called by phone and talked through the process of attaching the monitor. Once the patient had completed the recording, the monitors were then mailed back to the hospital for analysis using a recorded delivery postal system.
Our previous experience using this approach in the research setting has lent itself well to use in the COVID-19 pandemic. However, even though this approach has helped us ensure patients can obtain these investigations without having to visit the hospital, we have found that a minority of Holter monitors need to be repeated as a result of poor-quality recordings. The use of enhanced instructions and guidance to patients on fitting of Holter monitors could potentially help to minimise this, and our research team has found that a phone call to talk patients through this process can be helpful.
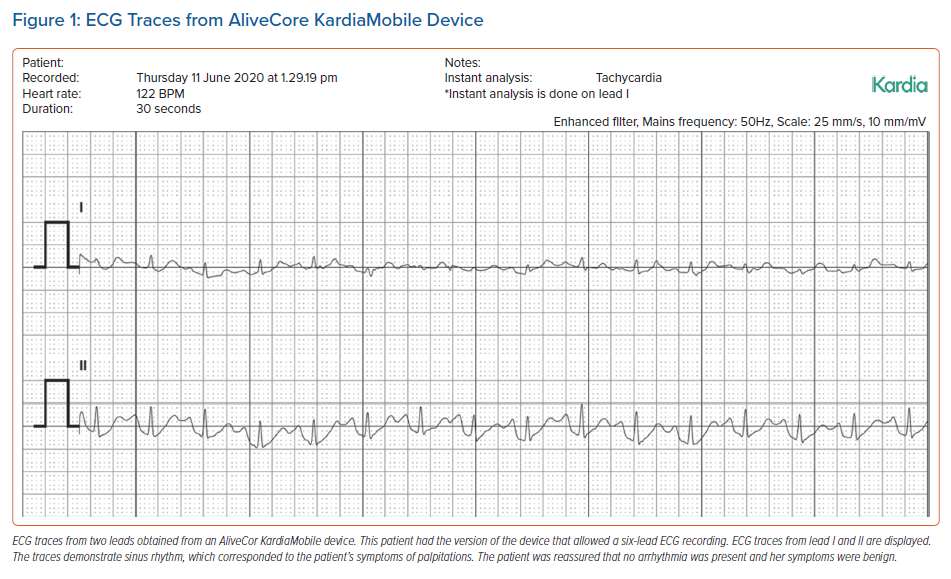
Holter monitoring is a useful diagnostic tool, but it can be difficult to capture an episode of symptoms using this, particularly if symptoms are infrequent. With this in mind, several hand-held monitoring devices that use smartphones have been developed – for example, AliveCor KardiaMobile or Apple Smart Watch – allowing patients to obtain an ECG trace at the time of their symptoms without being reliant on a monitor that is time dependent. These devices also have the advantage of allowing the patient to share the ECG traces with physicians via email. As a result, a clinical diagnosis can effectively be made through remote investigations. For example, the AliveCor KardiaMobile (Figure 1) has been shown to effectively identify AF and can do so in a larger proportion of patients compared with standard care, as shown in a randomised controlled trial.1,2
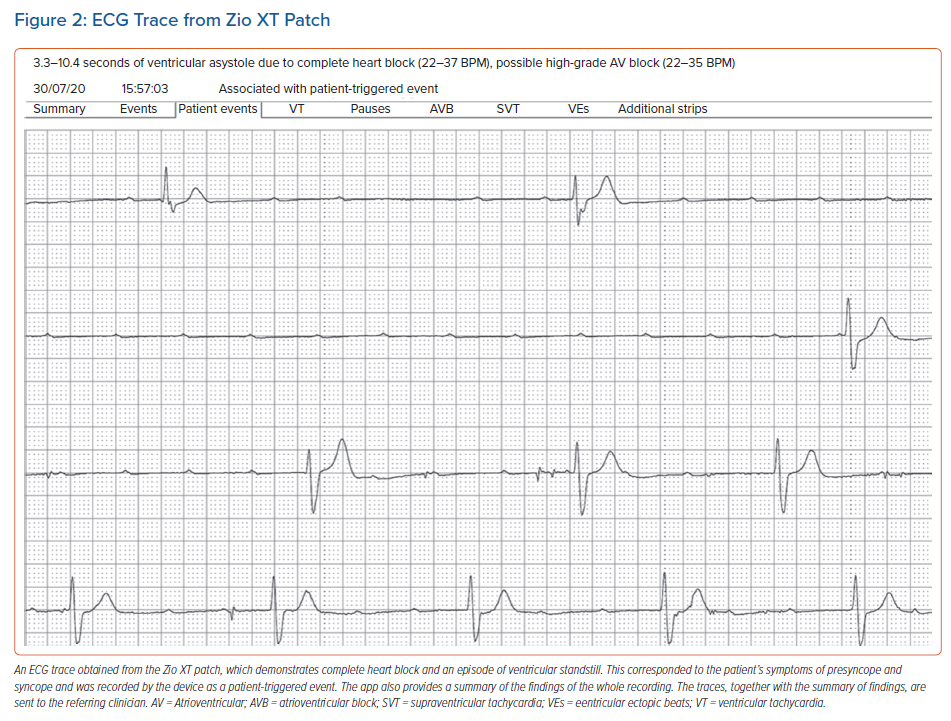
Even though these devices have clear advantages, not all patients are able to use them effectively, particularly older patients and those who do not have access to a smartphone or watch. In addition, for certain conditions, more detailed monitoring is required when investigating syncopal episodes. In these patients, alternative remote monitoring systems are available, such as the Carnation Ambulatory Monitor patch (BardyDx), consisting of a patch positioned over the sternum that allows ECG recording for 14 days. The patient can then transfer the data from the device onto a computer and share these with their clinician. These cardiac patches are also provided by other companies, such as the Zio XT patch by iRhythm Technologies (Figure 2), which has been compared to Holter monitoring and shown to be as good at detecting clinically significant arrhythmias.3 The main advantage of all of these devices is that the data can be readily shared between patient and clinician, providing a platform where remote investigations can be acted on promptly.
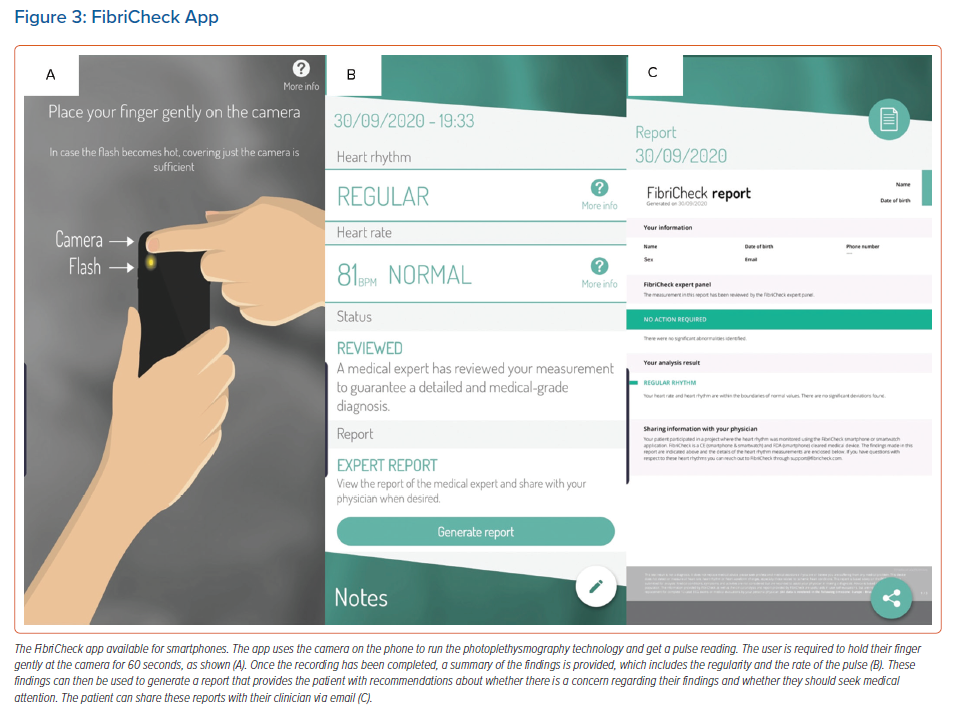
There are other devices available with the predominant focus on detection of AF. One of these devices is the FibriCheck app, which works through a smartphone app. This detects irregularities in heart rhythm that can be indicative of AF using validated photoplethysmography (Figure 3).4 FibriCheck was made available for free during the COVID-19 pandemic. The purpose of these devices is to detect episodes of AF, whether capturing episodes of symptoms, or screening patients without symptoms. Similarly to the other devices discussed, the findings from these devices can be readily sent to the clinician.
These devices have provided a leap forwards in terms of remote investigations, particularly for infrequent symptoms that are difficult to capture by conventional Holter monitoring, but this has relied largely on patients purchasing their own devices. Some patients are less willing or able to meet this cost. State-funded healthcare in the UK will not reimburse patients for monitoring equipment or reimburse hospitals for providing this to patients. Private medical insurers have begun to do so. However, the economics of this arrangement in the private and state sectors is not yet resolved.
Virtual Meetings
Multidisciplinary team meetings are an increasingly important part of medical decision-making. Virtual meeting platforms, such as Google Meet, Zoom Video Communications, Microsoft Teams and StarLeaf, are well suited to this purpose and are now used widely in the NHS. Experience gained during the pandemic has demonstrated benefits that will have a lasting impact on the way we practise. The ability to join meetings without the need to be physically present in the hospital provides the foundation for a more national and international forum to bring together key opinions on management of patients with complex problems. These meetings also provide fantastic educational opportunities and, indeed, clinical teaching sessions have evolved in the same way. It is likely that these platforms will be more readily used after the pandemic, in view of the benefits they bring.
Remote Clinic Follow-up
Remote clinic follow-up has been in place for several months at our centre, whereby all patients discharged after elective procedures are reviewed remotely via a phone consultation with arrhythmia nurse specialists, unless there is a clinical need for physician review in person. Approximately 250 patients are currently under remote follow-up at our centre. Remote clinic follow-up has several advantages; the time, expense and infection risk of a hospital visit are avoided. This is especially advantageous for those living far away, which can be a large proportion of patients in tertiary and quaternary centres. Remote follow-up also preserves outpatient facilities for patients needing physician-delivered care. This not only ensures shorter waiting times for patients to see physicians, but also allows longer follow-up for patients seen remotely as a result of the availability of this additional resource.
These clinics have taught us that patients can obtain effective post-procedural care without needing hospital visits. As symptoms are fundamental in determining the management of most arrhythmia conditions, phone consultations have been an effective way to obtain a patient history without being reliant on face-to-face consultations. Several apps have been launched to allow remote follow-up appointments. Ortus-iHealth is one such app that can be used by patients and clinicians to manage their outpatient care. This app in particular allows patients to get reminders for appointments, access their clinic letters, communicate with their clinician and give consent for procedures via a smartphone. The physician can use the app via a web portal. Such apps are already facilitating remote follow-up appointments at our centre and will no doubt continue to evolve.
Digital health technologies are expanding and are being used more widely during the COVID-19 pandemic.5 Their use in the remote management of arrhythmia patients in the context of the pandemic is supported by the Heart Rhythm Society clinical guidelines.6 Mobile health system technologies available on mobile phones can also be helpful for remote patient management and are widely used worldwide, particularly in the US.7,8 Mobile technologies for outpatient platforms are not as widely used at our centre. However, their use is likely to be incorporated into the on-going remote management of arrhythmia patients.
Remote monitoring has also been implemented in patients with COVID-19 using an automated text-messaging system.5 The Covid Watch combined automated twice-daily text message check-ins with a team of telemedicine clinicians available to respond 24/7 to escalations in patients’ needs. This is an alternative remote monitoring approach that could potentially also be expanded into areas of arrhythmia management.
Even though remote outpatient clinics have several advantages, particularly in the current climate, it is important to recognise some of the limitations of remote follow-up. A lot of available technologies and use of our existing experience with remote monitoring allowed us to effectively achieve remote monitoring during the pandemic, but several measures had to be taken to make this feasible. Firstly, all patients were contacted by secretaries prior to their clinic appointment and informed that their appointments were via phone rather than face-to-face. This rescheduling process required additional administration time. The running of these clinics required some adjustment. However, the time dedicated to face-to-face consultations was quickly directed towards phone consultations, which required limited adjustment to our services. The same time slots were used for phone appointments as for face-to-face clinics, so the volume of appointments offered was unaffected.
Care was taken to verify patient identification with phone calls. Where possible patient communication was kept within working hours to minimise intrusion. Patient preferences for communication, including text messages, WhatsApp and email, were considered, while highlighting to patients where gaps in data security might exist and where they may jeopardise their privacy. From a patient’s perspective, these appointments can make it difficult for relatives and next of kin to participate. They also limit clinical examination of the patient, which plays a particularly important role in those with underlying heart failure. The lack of face-to-face consultation can also affect the rapport and the doctor–patient relationship. Going forwards, using additional resources such as virtual meeting platforms and being even more reliant on community services could potentially help to minimise the impact of some of these limitations.
As in many UK centres, our pacemaker and device clinic follow-up has been moved, where possible, to a remote format. Dedicated administration time was required for the physiologists to arrange the remote clinic appointments and for patients to obtain a home monitor. All device checks since March have become remote monitoring downloads at 4–6 weeks post-implant rather than an in-person check.
Likewise, a large portion of subsequent follow-up for pacemakers, implantable loop recorders, ICDs and CRT devices has been moved to remote follow-up. Many centres were already using home monitoring devices for complex devices such as ICDs and CRT devices, but extending this to simple pacemakers has been a massive expansion. Remote monitoring of simple pacemakers has not been shown to be inferior to in-office follow-up, although only one manufacturer’s model has been assessed to date.9 At St Bartholomew’s Hospital, the number of patients with pacemakers on remote monitoring has increased 15-fold because of the COVID-19 pandemic. The total number of patients now on remote monitoring is around 6,500 patients. Some 1,500 of these patients are on remote monitoring because of the COVID-19 pandemic; around a 20% increase. As a result of the COVID-19 pandemic, the remote workload now consists of around 90–100 patients per day during the week and around 40 patients during the weekend. Although there may be a long-term saving with this approach, there is an up-front cost associated with remote monitoring, which hospitals have absorbed in the short term. Again, the economics of this approach are not fully resolved yet and device companies may adjust costs of home monitoring to facilitate the massive explosion in demand.
Further to this, remote device clinic follow-up does have limitations. For example, these appointments do not allow any alterations to the device parameters and functionalities. Concerns related to cybersecurity and liability are partly responsible for the lack of advancement in this area.10 With the changes in remote management these advances might follow.
Remote device clinic follow-up also does not enable physical wound reviews and so reviews of wound pictures at 4–6 weeks follow-up post-procedure was implemented to mitigate this. However, this is not practical for a large portion of the population, particularly older patients and those who do not have access to digital imaging or email technologies.
As a result of the sudden nature of the transition to remote follow-up, not all patients’ parameters have been programmed for this follow-up schedule and some patients did not have remote follow-up enabled on their device. This requires them to return to the hospital to be set up for remote follow-up. Remote monitoring does have the advantage of daily alert transmissions for arrhythmia and device function issues, which can be dealt with quickly. However, if these device alert settings are not personally tailored the burden of unnecessary transmissions can be drastically increased. With the introduction of the LINQ II (Medtronic) and Lux-Dx ICM (Boston Scientific) loop recorder, remote programming will help reduce this burden. Finally, in the UK, the remote reimbursement tariff is significantly lower than for a face-to-face appointment, providing no financial incentive for services to continue to adapt to this model in the long term. The main incentive is to reduce the risk to patients and staff of contracting COVID-19 but, the longer-term motivation will be to have a better, more efficient and flexible service.
Conclusion
The COVID-19 pandemic has resulted in a radical, and probably permanent, change in the way that we deliver outpatient care. Our previous experience in remote review and the available technologies for monitoring have allowed us to conduct the majority of outpatient care without obviously compromising quality or safety, although the precipitous nature of change has meant that this assertion is largely untested. We have highlighted some of the benefits and limitations of remote care for arrhythmia patients. It is expected that technology will evolve to address these limitations and that new funding models will be developed, reflecting the radically altered landscape.
Clinical Perspective
- The coronavirus disease 2019 pandemic has resulted in a radical, and probably permanent, change in the way we deliver outpatient care.
- Our previous experience with remote monitoring and available technologies for monitoring have allowed us to conduct the majority of outpatient care without obviously compromising quality or safety.