The field of AF has had to contend with an evolving landscape following the publication of the Substrate and Trigger Ablation for Reduction of Atrial Fibrillation Trial Part II (STAR AF II) trial. This session focused on persistent AF and the issues regarding how best to treat it. Instead of examining pulmonary vein isolation (PVI) alone, speakers critically questioned the current evidence and looked beyond the pulmonary veins as therapeutic targets.
Limitations of the Current Definitions of Persistent AF
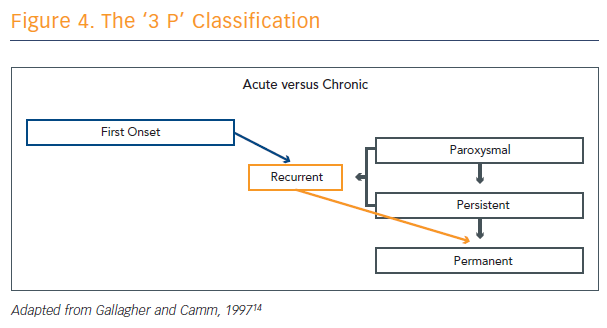
The term ‘persistent AF’ was first used in 1997.14 The ‘3 P’ definition (see Figure 4) has been in use since then and has not changed drastically over the intervening years. Prof John Camm from St George’s, University of London and Imperial College London, UK, was one of the authors who helped create the definition. At the time, they were looking for a ‘P’ between paroxysmal and permanent, building on the then-evolving discussion around acute and chronic. The co-authors split the concepts into first-onset (paroxysmal), recurrent (persistent) and permanent.
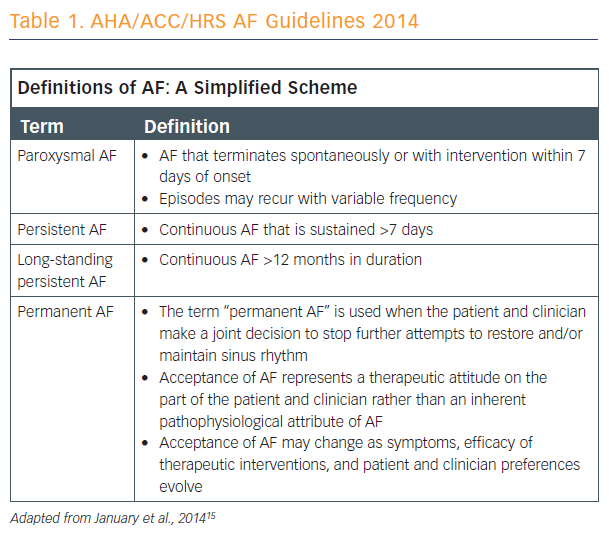
The concept of long-standing persistent AF was introduced in the 2014 guidelines. Persistent AF is defined as continuous AF sustained for greater than 7 days and long-standing persistent AF is continuous AF that is longer than 12 months in duration.15
Prof Camm said that we cannot look at persistent AF without considering the definitions of paroxysmal AF (a shorter-duration arrhythmia), while long-standing and permanent AF are termed continuous arrhythmia. Paroxysmal AF can be described as self-terminating – within 48 hours in most cases – although some paroxysmal AF can last up to 7 days. This can be further broken down into short episodes of paroxysmal AF, episodes of paroxysmal AF that terminate soon, and episodes of paroxysmal AF that terminate after a long time. Persistent AF requires induced termination, which is sometimes divided into earlier termination and later episodes of termination.
New concepts are evolving these definitions within AF in ways that make the terminology more precise, if somewhat more complicated (see Table 1). This is important because of the progressive nature of AF and because the definitions used are critical for dictating future treatment intention. There are also differences in hazard ratios depending on how the patient condition is stratified, even within the different levels of persistent and paroxysmal AF.
The temporal classification of a single AF episode is clinically useful, but definitions are numerous and unclear. The temporal pattern has been used in the clinic and in clinical trials to choose therapy or to stratify patients, but the temporal classification must be replaced, improved or supplemented to facilitate treatment decisions. Multidimensional classifications of AF (e.g. CHADS-VASC, EHRA score, 7P classification), and clinical- and device-derived AF classifications may be helpful to supplement the definitions, but more work needs to be done in these areas.