Implantable cardiac devices such as implantable cardioverter- defibrillators (ICDs) and cardiac resynchronisation therapy (CRT) devices lead to improved survival and better clinical outcomes in appropriately selected patients with heart failure (HF) with a reduced ejection fraction (EF). Although there are significant sex differences in the aetiology, pathophysiology and clinical course of HF, clinical practice guidelines for cardiac device therapy are not sex-specific and are based on clinical trials where the majority of patients enrolled were men. In this review, we explore sex differences in clinical outcomes and utilisation of ICDs and CRT and explore the reasons for these disparities.
Implantable Cardioverter-Defibrillators
The annual incidence of sudden cardiac death (SCD) in the US is estimated to be 300,000 to 450,000.1 A major risk factor for SCD is HF with reduced EF. There have been several large randomised controlled studies that have demonstrated a mortality benefit from ICDs in eligible patients for both primary and secondary prevention of SCD. However, under-representation of women in these trials has made it somewhat difficult to determine the sex-specific survival benefit of ICD therapy.
Evidence for the Use of ICD Therapy for Primary and Secondary Prevention of SCD
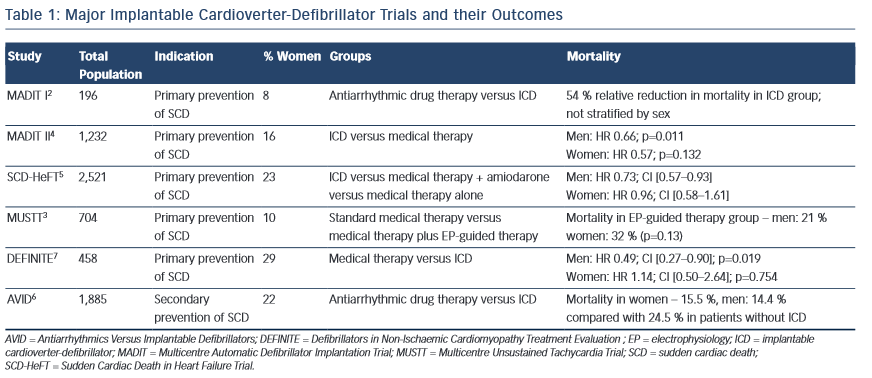
The Antiarrhythmics versus Implantable Defibrillators trial (AVID), Cardiac Arrest Study Hamburg (CASH) trial and the Canadian Implantable Defibrillator Study (CIDS) all showed a survival benefit from ICDs in patients who had already survived a potentially life-threatening ventricular arrhythmia. Multiple primary prevention trials (the Multicentre Automatic Defibrillator Implantation Trial [MADIT I], the Multicentre Unsustained Tachycardia Trial [MUSTT] and MADIT II) all showed improved outcomes with ICD therapy in patients with a history of myocardial infarction (MI) and significant left ventricular (LV) dysfunction.2–4 Similarly, in the Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT), patients with LVEF <35 % and at least New York Heart Association (NYHA) class II HF had better survival with ICDs compared with medical therapy plus amiodarone or medical therapy alone.5 The SCD-HeFT trial included patients with non-ischaemic cardiomyopathy, which further expanded the patient population eligible for ICD therapy. Table 1 lists the major ICD clinical trials. Of note, in all of these trials, less than 25 % of the total population enrolled were women.
Sex Differences in Outcomes with ICD Therapy
Sex Differences in ICD Therapy for Secondary Prevention of SCD
Curtis et al.6 analysed a 5 % national sample of patients from the US Centers for Medicare & Medicaid Services eligible for ICD therapy and found that, in the secondary prevention ICD cohort, there was a statistically significant mortality benefit for both sexes even after adjustment for other factors.
Sex Differences in Primary Prevention ICDs
In the MUSTT trial,3 a total of 301 women were enrolled, and they constituted 10 % (68) of the randomised patients and 16 % (233) of those followed in the registry. Overall, there was no statistically significant difference in mortality between men and women in the electrophysiology (EP)-guided therapy group (21 % versus 32 %; p=0.13) or in the registry (20 % versus 27 %; p=0.15). However, there was a trend towards increased mortality in women, although the trial did not have sufficient power to detect gender differences due to the small number of women enrolled.
In MADIT-II, 1,232 patients with ischaemic cardiomyopathy were enrolled of which 192 (16 %) were women.4 Patients received ICDs versus standard medical therapy, with a total of 119 women receiving ICD therapy. Women were noted to have more advanced HF, as well as a higher incidence of hypertension, diabetes and left bundle branch block (LBBB). The 2-year overall mortality rate as well as the rates for SCD were similar between men and women in the medical therapy arm of the trial. The hazard ratios for ICD effectiveness after adjusting for clinical covariates were similar for men and women (men: HR 0.66; p=0.011; women: HR 0.57; p=0.132). The interaction between gender, mortality and ICD therapy was not significant (p=0.72).
SCD-HeFT enrolled a total of 2,521 HF patients (588 [23 %] women) and included patients with both ischaemic and non-ischaemic cardiomyopathy.5 Patients were randomised to amiodarone, placebo or ICD in a 1:1:1 manner, with 185 women receiving an ICD. A post-hoc analysis of the trial revealed a mortality benefit for men but not for women for the primary prevention of SCD. However, it was noted that women had a much lower overall mortality risk compared with men (HR 0.68; 95 % CI [0.55–0.84]; p=0.001). In addition, the trial was not adequately powered to detect sex differences, as the number of women enrolled was so low. Similarly, the Defibrillators in Non- Ischaemic Cardiomyopathy Treatment Evaluation (DEFINITE) trial reported a mortality benefit for men in the ICD group but not women (men: HR 0.49; 95 % CI [0.27–0.90]; p=0.019; women: HR 1.14; 95 % CI [0.50–2.64]; p=0.754).7 The study was not powered to detect sex differences, and only 63 women were randomised to an ICD (total number of patients in the study was 458, including 132 women).
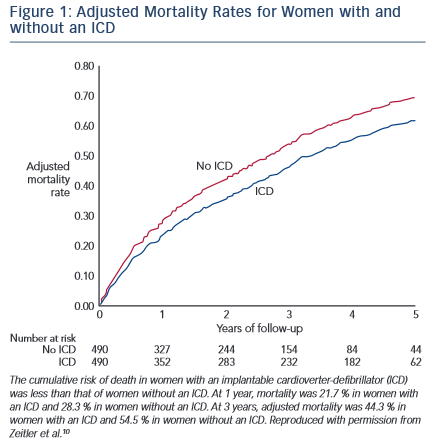
MacFadden et al.8 followed 5,213 Canadian HF patients who received primary and secondary prevention ICDs for up to 1 year. Of the 921 women who received ICDs for primary prophylaxis and 367 who received ICDs for secondary prophylaxis, they found no difference in mortality between men and women. However, women were less likely to receive appropriate ICD shocks. Another observational study of 582 patients (291 men and 291 women propensity matched based on age, EF, indication for ICD therapy and ischaemic versus non- ischaemic cardiomyopathy) found no difference in mortality rates between men and women.9 Zeitler et al.10 analysed data from the National Cardiovascular Data Registry (NCDR) ICD Registry, the Get With The Guidelines-HF [GWTG-HF] database, and the Centers for Medicare & Medicaid Services on women eligible for a primary prevention ICD. There were 490 women with primary prevention ICDs who were matched with 490 women without an ICD but who were eligible for a primary prevention ICD. After a median follow-up of 4.6 years, women with ICDs had better survival than women without ICDs (HR: 0.79; 95 % CI [0.66–0.95]; p<0.013) (see Figure 1). Further statistical analyses revealed that the clinical effectiveness of ICD therapy did not vary by sex. Similarly, the Registry to Improve the Use of Evidence-Based Heart Failure Therapies in the Outpatient Setting (IMPROVE HF) study found that ICD and CRT therapy was associated with a similar mortality benefit in both men and women with HF eligible for device therapy.11
Curtis et al.6 analysed a 5 % national sample of patients from the US Centers for Medicare & Medicaid Services eligible for ICD therapy and found that unadjusted analyses showed a significant survival benefit for women in the primary prevention ICD cohort. However, this finding was no longer significant after adjustment for confounding factors.
Several meta-analyses have attempted to look into sex-specific outcomes with ICDs, especially for primary prevention of SCD, with conflicting results. In a recent meta-analysis, Ghanbari et al.12 combined data from five major primary prevention trials including MUSTT, MADIT II, SCD-HeFT, DEFINITE and the Defibrillator in Acute Myocardial Infarction Trial (DINAMIT) trial. A total of 3,810 men and 934 women were included in the analysis. A mortality benefit was seen in men receiving ICD therapy compared with medical treatment (HR 0.78; 95 % CI [0.70–0.87]; p<0.001) but not in women (HR 1.01; 95 % CI [0.76–1.33]; p=0.95).
Another recent meta-analysis by Santangeli et al.13 analysed data from five major trials (MUSTT, MADIT-II, SCD-HeFT, DEFINITE and the Comparison of Medical Therapy, Pacing and Defibrillation in Heart Failure [COMPANION] trial, the last of which was a CRT trial). These trials enrolled 7,229 patients of which 23 % (1,630) were women. Women had a similar overall mortality rate, although only men had a statistically significant mortality benefit with prophylactic ICD therapy (men: HR 0.67; 95 % CI [0.58–0.78]; p<0.001; women: HR 0.78, 95 % CI [0.57–1.05]; p=0.1). Women also experienced lower rates of appropriate ICD interventions (HR=0.63; 95 % CI [0.49–0.82]; p<0.001).
Under-representation of women in cardiac device trials is a significant problem, with women constituting <25 % of the total enrolled population. The resulting HRs for mortality benefit with ICD therapy in women have wide confidence limits, indicating that the studies were underpowered to detect a significant mortality benefit with ICD therapy in women.
There are other differences in outcomes with ICD therapy between men and women beyond mortality. Men with coronary artery disease (CAD) in whom ICDs have been implanted have more ventricular tachycardia/ventricular fibrillation (VT/VF) events as well as more ICD shocks and electrical storms than women.14 Lampert et al.15 reviewed the records of 340 men and 59 women with CAD who received an ICD and followed them for 30±22 months. They found that 52 % of the men experienced sustained VT or VF requiring ICD therapy (p<0.01) compared with 34 % of the women. Overall, men also experienced more VT/VF events than the women in the study.
Myocardial scarring post-infarction is more often seen in men, and ischaemic scars are frequently the substrate for sustained monomorphic VT. Other studies have demonstrated that men presenting with out-of- hospital sudden cardiac arrest are more likely to have VT/VF versus women (41 % versus 30 %). Women are more likely to have asystole (8.8 versus 7 %) or pulseless electrical activity (24 versus 18 %) than men.16 These findings from various studies could suggest that SCD in women is more often due to non-shockable arrhythmias compared with men. No significant difference has been found in the incidence of VT among men and women with non-ischaemic dilated cardiomyopathy.17
There have also been studies looking at sex differences in complications following cardiac device implantation. Peterson et al.18 identified 161,470 patients from the NCDR ICD Registry, of which women constituted around 27 % (43,655) of the cohort. Women were more likely to have HF, non-ischaemic cardiomyopathy, advanced NYHA class and were more likely to receive CRT-defibrillators (CRT-D) compared with men. Women had a higher in-hospital adverse event rate after ICD implantation than men (4.4 versus 3.3 %; p<0.001). In particular, peri-procedural complications were more common in women, although there was no difference in in-hospital mortality between men and women.
Sex Disparities in ICD Utilisation
Hernandez et al.19 analysed data from the GWTG-HF programme and studied 13,034 patients with HF who were eligible for ICD therapy. The study revealed that while around 44 % of eligible (white) men received ICDs, only around 28 % of eligible women received ICD therapy. In addition, after adjustment for patient-related factors, the odds ratios for ICD use were 0.73 for African-American men, 0.62 for Caucasian women and 0.56 for African-American women compared with white men. These differences were not attributable to the proportions of women and African–American patients at participating hospitals or to differences in the reporting of LVEF. The study by Curtis et al. mentioned previously showed that only 8.6 per 1,000 women received an ICD compared with 32.3 per 1,000 men within 1 year of known eligibility for a primary prevention ICD. The rates of ICD implantation for secondary prevention of SCD were also equally disproportionate in women (38.4 per 1,000) compared to men (102.2 per 1,000).
Over the past few years there have been ongoing efforts to improve utilisation of implantable cardiac device therapy in eligible female patients. The IMPROVE HF20 study evaluated whether a programme to provide clinical decision-making support tools and educational materials to healthcare providers would lead to similar improvements in adherence to clinical practice guidelines for both male and female patients. This was a prospective study where high-risk patients with HF with reduced EF (<35 %) eligible for treatment with an ICD, CRT or several other guideline-recommended therapies were identified and hospitals were provided with clinical algorithms, pocket cards, patient educational materials and patient assessment forms and were followed for 24 months. The study included a total of 15,170 patients of whom 4,383 (28.9 %) were women. At the end of 2 years, rates of ICD use went up from 40–50 % to 75–80 % and CRT use from 35–40 % to 65–75 % in both men and women. Thus, providing clinical decision-making support and education can lead to better ICD therapy utilisation in eligible patients irrespective of sex. Similarly, Al-Khatib et al. analysed 11,880 patients enrolled in the GWTG-HF program for trends in ICD implantation rates over the past decade and found that with the implementation of the GWTG-HF program, rates of ICD implantation went up overall (around 30 % in 2005 to 42 % in 2007). The greatest increase in ICD use was seen in African–American women (23.3% increase), a group in whom the use of implantable cardiac devices has been extremely low compared with white men.21
Cardiac Resynchronisation Therapy
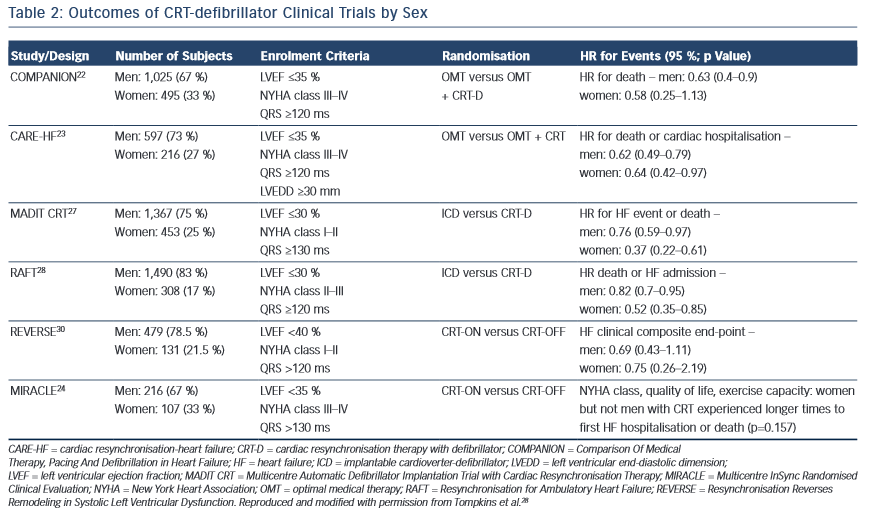
Severalstudies,includingCOMPANIONandtheCardiacResynchronisation- Heart Failure (CARE-HF) study, have demonstrated a significant mortality benefit with CRT in eligible patients.22,23 In addition to these studies, trials such as the Multicentre InSync Randomised Clinical Evaluation (MIRACLE), Pacing Therapies in Congestive Heart Failure (PATH-CHF), and Multisite Stimulation in Cardiomyopathies (MUSTIC) showed that CRT therapy in HF patients led to significant improvements in clinical symptoms, NYHA class and quality of life.24–26 Table 2 lists the major CRT trials and the percentage of women enrolled in each trial.
Sex Differences in Outcomes with CRT Therapy
Compared with the ICD trials, CRT trials have had a higher number of female patients (around 30 %). However, considering that in the US the prevalence of HF is similar in both sexes,1 women have still been significantly underrepresented in CRT trials.
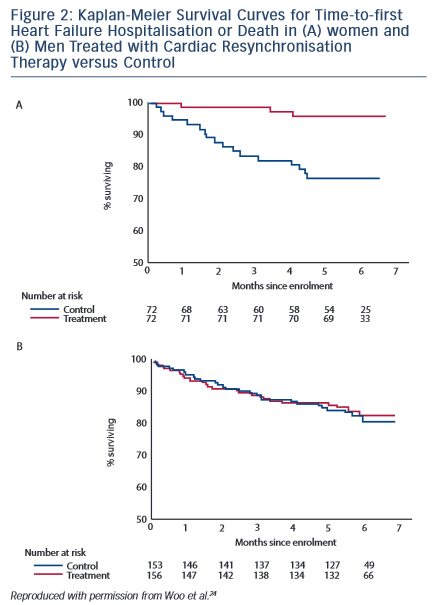
The MIRACLE trial enrolled 453 patients with HF with reduced EF (<35 %), NYHA class III or IV and QRS >130 ms and randomised them to CRT or the control group. Women constituted 36 % of the total enrolment (144/453). Improvements in both clinical status and cardiac function were seen in the CRT group. Woo et al.24 analysed eight pre-specified subgroups in the MIRACLE study, including sex, for differences in response to CRT. They found that compared with control subjects, women but not men with CRT experienced longer times to first HF hospitalisation or death (see Figure 2).
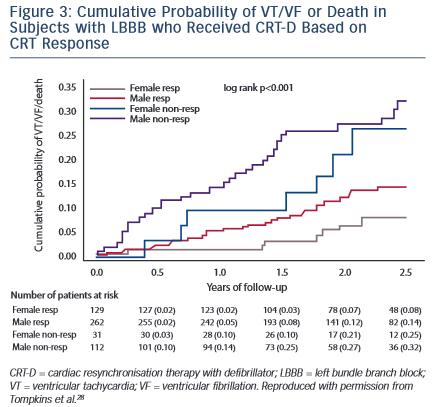
The Multicentre Automatic Defibrillator Implantation Trial with Cardiac Resynchronisation Therapy (MADIT-CRT) enrolled 1,820 patients with NYHA class I and II symptoms, LVEF <30 % and QRS >130 ms, of whom 453 were women.27 Patients were randomly assigned to CRT-D or ICD alone. Patients in the CRT-D arm experienced a 34 % reduction in the combined endpoint of HF or death. The study pre-specified an analysis by sex and found that the primary outcome of HF or death was seen in 29 % of the women with ICDs and 11 % of those with CRT-D compared with 25 % of men with ICDs and 20 % with CRT-D (women: HR 0.31; p<0.001; men: HR 0.72; p<0.01). The short-term sex-specific outcomes demonstrated a statistically significant reduction in mortality in women (HR 0.28; 95 % CI [0.10–0.79]; p<0.02) but not in men (HR 1.05; 95 % CI [0.70–1.57]; p=0.83). Furthermore, this mortality benefit was seen in women with a QRS duration >150 ms and in women with LBBB but not in men (see Figure 3).28 More recently, Biton et al.29 presented the results of long-term sex-specific outcomes in the MADIT-CRT population with LBBB. A total of 1,281 patients were included in this analysis, including 394 women and 887 men. Both men and women experienced a significant mortality benefit with CRT-D versus ICD only. However women had a significantly greater reduction in HF only and HF or death with CRT-D compared with men.
The COMPANION and CARE-HF trials both demonstrated improvements in time-to-first hospitalisation or death in patients with advanced HF with CRT.22,23 The COMPANION trial enrolled 1,520 patients with NYHA class III or IV HF and compared CRT with either a pacemaker (CRT-P) or a defibrillator (CRT-D) to optimal medical therapy. Women constituted around 30 % of the total population, and there was a statistically significant reduction in the risk of the combined primary endpoint of death or hospitalisation for both men and women.
The Resynchronisation Reverses Remodeling in Systolic Left Ventricular Dysfunction (REVERSE) trial evaluated the effects of CRT on the clinical course and LV function in patients with mild HF.30 There were 684 patients enrolled in the trial, with women constituting 20 % of the total enrolment. Patients were randomised to CRT or the control group and a pre-specified analysis of 419 patients with CRT devices turned on was performed. Patients in the CRT-ON group were followed for an additional 5 years, and on multivariable analysis it was found that there was a significant survival benefit for patients with CRT-D devices compared with the control group, with the mortality benefit being larger for women than men.
Xu et al.31 retrospectively evaluated 728 patients who received CRT with the aim of detecting sex differences in CRT effectiveness. Women constituted 22.8 % (166) of the total sample and had a statistically significant improvement in NYHA class that was not seen in men (p=0.009). A greater improvement in LVEF was also seen in women compared with men. Other prospective studies have demonstrated that women experience better survival, longer event-free survival from death/HF hospitalisation as well as significantly better improvements in NYHA class, LVEF and LV reverse remodelling with CRT compared to men.32 Using a Cox proportional hazards model, it was also shown in the above-mentioned study that female sex was an independent predictor of survival regardless of age, LVEF, QRS duration, type of CRT device and NYHA class.
Loring et al. also showed that LBBB was associated with a significantly better survival rate in women compared with men treated with CRT.33 In this study of 144,642 CRT recipients, women with LBBB experienced a 26 % reduction in mortality (HR 0.74; 95 % CI [0.71–0.77]), while men experienced a reduction of 15 % (HR 0.85; 95 % CI [0.83–0.87]) after adjusting for confounding factors. An improvement in echocardiographic parameters in women with CRT was also observed in a study by Lilli et al. They followed 195 patients for 12 months after they received CRT and found that women showed a greater benefit with CRT in the form of decreased LV end diastolic volumes and higher LVEF compared with men.34 More recently, the IMPROVE HF trial showed that both men and women with ICD/CRT-D derived a significant mortality benefit (men OR, 0.67; 95 % CI [0.49–0.92]; p=0.0133; women OR 0.53; 95 % CI [0.31–0.91]; p=0.0227), and this benefit persisted after adjusting for age.11
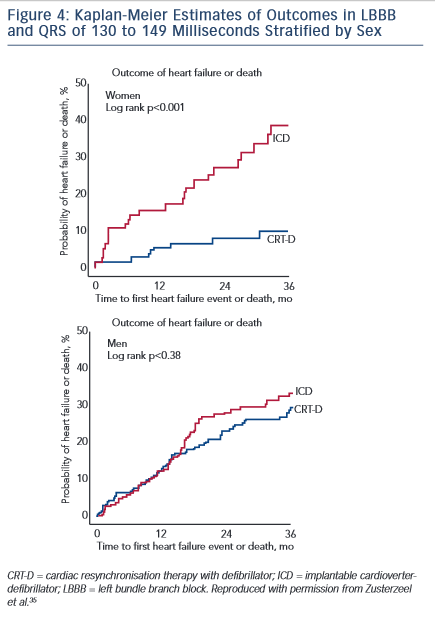
Zusterzeel et al.35 combined patient data from three major CRT-D versus ICD trials (MADIT-CRT, Resynchronisation for Ambulatory Heart Failure Trial [RAFT] and REVERSE) to conduct a post-hoc meta-analysis evaluating sex-specific outcomes with CRT. The final analysis included 4,076 patients, of which 22 % were women. Women with mild HF, LBBB and a QRS duration of 130–149 ms showed a 76 % reduction in mortality with CRT-D (HR 0.24; 95 % CI [0.06–0.89]), with no similar benefit in men with similar findings (see Figure 4).
The relationship between sex and response to CRT with varying QRS durations in patients with LBBB was further studied by Varma et al.36 Patients with NYHA class III/IV HF, non-ischaemic cardiomyopathy and LBBB with a CRT device were followed for a period of 2 years. A total of 212 patients were enrolled of which 49.5 % (104) were women. The overall positive response rate in both sexes was 76 % in those with a QRS >150 ms, and 58 % in those with a QRS <150 ms. However, women had a higher response rate than men at a QRS <150 ms (86 % in women versus 36 % in men; p<0.001). These studies indicate that the relationship between QRS duration and response to CRT is different between men and women.
One reason why women might benefit more from CRT than men at shorter QRS durations may be that women normally have shorter QRS durations than men. Thus, any particular degree of QRS prolongation is relatively longer in women compared with men and may indicate greater dyssynchrony. By not considering sex-related differences in response to CRT, there is a possibility that practice guidelines might exclude female patients with shorter QRS durations who would benefit from CRT.
Sex Disparities in Cardiac Resynchronisation Therapy Utilisation
Women with HF are usually older than men, and they are more likely to have HF with preserved EF compared with men. They are also more likely to have non-ischaemic cardiomyopathy and are more often diabetic and hypertensive. As eligibility for CRT is based on EF (EF <35 %), many women with HF with preserved EF will not be candidates for CRT despite having a worse NYHA class.
Despite the overall prevalence of HF in women being slightly less than that of men, a study sponsored by the Agency for Healthcare Research and Quality revealed that hospital admissions for HF exacerbations or HF-related complications have been higher among female HF patients than male patients. This trend has been consistent over the past three decades.37 Data on new CRT implantations from 2002 to 2004 extracted from the Healthcare Cost and Utilisation Project showed that the total number of CRTs implanted increased significantly (2,590 CRT devices implanted in 2002 and 34,803 in 2004). An increase in the use of CRT was seen both in women and men; however, the increase was significantly less in women compared with men (women: 659 in 2002 versus 11,286 in 2004; men: 1,931 in 2002 versus 42,196 in 2004). This disparity remained even after adjusting for the lower incidence of CHF in women.
Various studies have identified female sex as a positive predictor of response to CRT. Leyva et al.38 studied long-term clinical outcomes after CRT implantation in 550 patients, of which 122 (22 %) were women. A Cox proportional hazards analysis showed that women had better survival from death due to any cause as well as cardiovascular death. They also had a lower incidence of the combined endpoint of cardiovascular death/HF hospitalisations. A greater increase in LVEF and a greater reduction in LV end-systolic volume were seen in women compared with men. These benefits were independent of QRS duration, NYHA class, LVEF, age and other comorbidities.
Despite a clear mortality benefit seen with CRT in women, this life- saving therapy is still significantly underutilised in women as noted above. As demonstrated in the IMPROVE HF study, a significant improvement in CRT utilisation was seen in both men and women when clinical decision-making support and information were provided to physicians and patients.
Conclusion
There is ample evidence that ICDs and CRT provide significant benefit in terms of mortality and other important clinical outcomes in patients eligible for these devices. However, the majority of patients enrolled in these trials have been men. Thus, determination of sex-specific mortality and clinical outcomes has often not been possible owing to the low numbers of women enrolled. There are differences in cellular electrophysiological properties, autonomic modulation and hormonal effects on the expression of ion channels as well as the arrhythmogenic substrate between men and women that may explain the lower incidence of life-threatening arrhythmias in women compared with men. However, there is enough evidence regarding the survival benefit with ICD therapy in both sexes that recommendations as to which patients should receive ICD therapy do not vary by sex. With CRT, women benefit more than men in general, likely because of both a higher incidence of non-ischaemic cardiomyopathy and relatively greater dyssynchrony for any particular QRS duration. Thus, the rate of CRT use in women should be at least equal to that in men. In fact, current practice guidelines may be too restrictive in their recommendations as to the QRS duration that warrants consideration of CRT in women, given that the recommendations were based largely on outcomes in men in the clinical trials.
Eligible female patients are less likely to receive both ICD and CRT therapy, although the guidelines clearly state that these life-saving therapies should be offered to all patients irrespective of sex. It has also been demonstrated in multiple performance improvement initiatives that this sex-based disparity can be significantly reduced with favourable outcomes for both sexes. There is still a large gap between the number of patients who are eligible for implantable cardiac devices and those who receive it, and this gap is especially wide in women. A concerted effort to enroll more women in cardiac device trials and offer eligible patients implantable cardiac devices regardless of sex is necessary.